Is Chronic Fatigue Adrenal Fatigue?
Identifying the cause of chronic fatigue is often a challenge in medicine. If obvious medical conditions like heart disease, diabetes, autoimmune conditions are ruled out most physicians assume fatigue is a symptom of depression Though that can be the case, in the majority of medical visits where fatigue is the main complaint an underlying cause can be identified using the concepts of integrative medicine
Fatigue is one of the most common reasons for medical evaluation, with up to 35% of all primary care visits for problems of fatigue and tiredness. One confusing area is the role adrenal function plays in fatigue. Many endocrinologists dispute the existence of adrenal fatigue except in cases of Addison’s disease (a rare auto-immune destructive condition) On the other hand it is common to hear non MD practitioners make a diagnosis of adrenal exhaustion as a frequent cause of fatigue.
Actually both ideas are accurate. The adrenal gland makes cortisol, the most important adaptive and stress hormone which controls many of the functions which effect energy production. Cortisol maintains blood sugar, fights inflammation and allergies and helps us survive stressful challenges. Cortisol is one hormone that we can not live without, allowing us to survive the challenges our distant ancestors faced with struggles for survival. However, with the type of chronic low level on going stress we face today, the adrenal response can become dysfunctional leading to fatigue and other symptoms.
In actuality, the story is more complicated than just the adrenal glands letting us down. The adrenals takes direction from the pituitary gland (the master gland of the hormone system) which secretes ACTH (adrenocorticotrophic hormone) that stimulates cortisol production from the adrenal gland. The pituitary takes direction from the hypothalamus which makes CRH (corticotrophic releasing hormone) that tells the pituitary to make ACTH. The hypothalamus function is influenced by the midbrain the seat of emotional memory. It is this complex interface between emotions, trauma, memories and one’s current state, both mentally and physically that determines cortisol output. The idea of adrenal burnout, implying that the adrenal gland itself is somehow damaged or unable to produce enough cortisol is not what actually happens. Let’s take a deeper look.
Adrenal Fatigue and Stress
Both emotional and physical stressors, as well as a history of trauma, including childhood events, can effect the adrenal function and the stress response throughout life. The midbrain (the amygdala and hippocampus), the seat of control of the adrenal system, stores memories of trauma and stress. This part of the brain is the crossroad between emotions like fear, traumatic events, and the function of the endocrine system including the adrenal production of cortisol and 30 other hormones. When long term stress occurs, unlike other physiologic functions (homeostatic), the stress response often stays up-regulated even after the stressful situation is resolved. This is called allostatic load and leads to chronically elevated cortisol and adrenal response, even when not needed. Eventually, in most people, the brain will reduce the excess allostatic cortisol production as a protective mechanism to prevent the serious consequences of elevated cortisol-weight gain around the middle, diabetes, immune suppression leading to greater cancer risk, heart disease and depression and anxiety. When cortisol responsiveness is lowered the outcome is worse fatigue, poor exercise tolerance, increased food and airborne allergies and reduced capacity to adapt to new stressors, major of minor (often seen in PTSD). This is what many call adrenal burnout.
How is adrenal and chronic fatigue diagnosed?
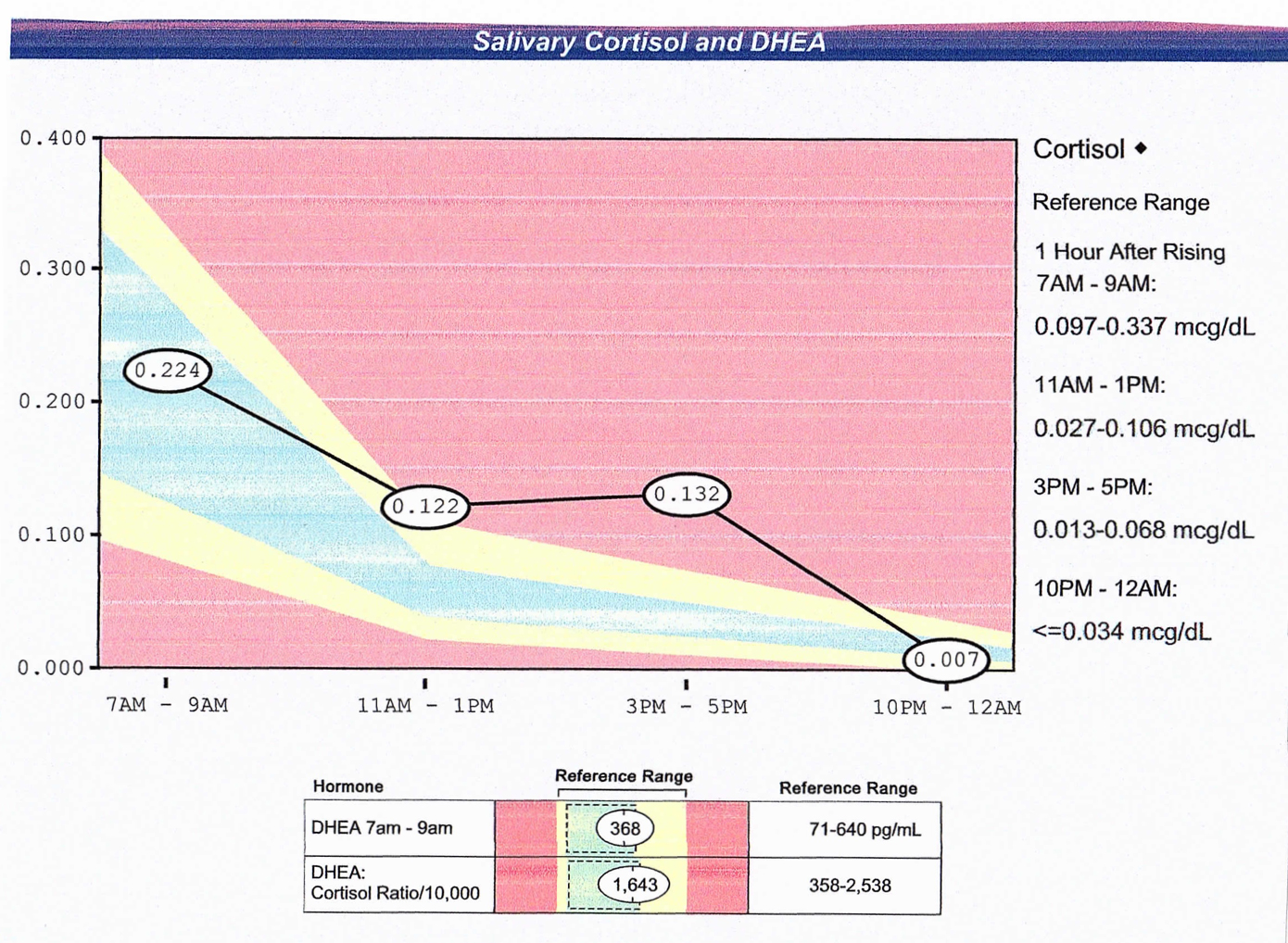
To assess the adrenal function directly we use salivary cortisol tests, as well as blood and urine tests, to establish the level of cortisol production. This determines the stage of adrenal and midbrain dysfunction. Cortisol production normally ramps up during sleep, with the peak production at 8 am,and gradually reduces throughout the day with the lowest level before sleep. A common pattern I see with long standing stress and fatigue, shows a low cortisol level in the morning with elevated night time levels. This if often seen with a person fatigued during the day but unable to let down and relax at night often with insomnia. Tired and wired, these people often use coffee in the am for energy and alcohol at night to relax. Both contribute to adrenal dysfunction.
The fatigue from lowered adrenal response is experienced through these symptoms:
- Exercise intolerance, especially with weight training
- Increased inflammation of muscles, joints, the GI tract
- Depression or anxiety often not related to situation
- Food allergies and intolerance
- Poor concentration and memory
- Hypervigilance to any perceived risks, often ‘tired and wired’
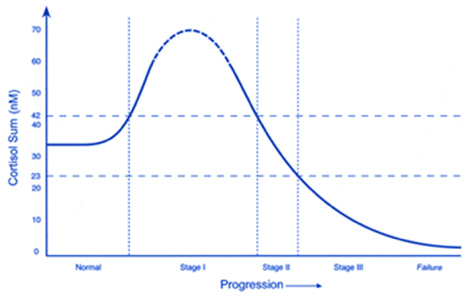
Graph of phases of cortisol production in long standing stress, with the outcome adrenal deficiency and chronic fatigue.
Remedies for Adrenal Fatigue
Recovering from fatigue that involves the midbrain and adrenal function requires looking at the whole person and the stress load they are dealing with. Proper diet is critical in resetting adrenal function including high fiber, low inflammation foods, avoiding food allergies and gluten and eating the right fats. (see The Adaptation Diet) Specific stress management techniques including meditation, proper individualized exercise as well as supplements for sleep issues are all part of the fix.
Most specifically to reset the cortisol function, the use of adaptogenic botanicals (adaptogens are botanicals that improve the function of the the hypothalamic-pituitary-adrenal axis and include rhodiola, ashwaghanda, eleutherococcus, ginseng, licorice root) and nutrients are needed. I have found high dose omega 3 marine lipids (EPA-DHA), flaxseed powder and phosphatidyl serine to be very important. To provide the best of the adaptogens in one supplement, I have developed the Cortisol Control Formula™ combining the adaptogenic herbs with anti-inflammatory botanicals to optimize adrenal function. In addition, minerals such as magnesium (especially magnesium threonate) and vitamins like B5 and B6 all support normal adrenal function and lead to higher energy.
Chronic fatigue can also be also be triggered by a variety of events in addition to long standing stress
Patients I see often have the onset of fatigue after a viral infection, environmental exposure such as mold in a water damaged home or workplace, travel borne illness like diarrhea from a parasite or bacteria. The first question I always ask is what events preceded the onset of the fatigue. In susceptible individuals (determined by genetic testing) the immune response to infections or toxins like mold, leads to a state of chronic inflammation called CIRS (Chronic Inflammatory Response Syndrome) Once this occurs it leads to chronic fatigue as well as other symptoms such as joint pains, headaches, depression and digestive problems.
In addition to adrenal/midbrain based fatigue, there are other common causes of tiredness and lethargy that are best evaluated with an integrative medicine approach. The following is a list of other causes for fatigue, tiredness and lethargy (I am not including conditions such as diabetes, cancer, heart disease, auto-immune disorders which all need to be ruled out as obvious causes of fatigue) :
Causes of Chronic Fatigue beyond the Adrenal Function
Chronic fatigue often involves other hormones in addition to cortisol. Through blood tests we assess thyroid, sex hormones including estrogen and progesterone in women and testosterone and DHEA in both women and men. Nutritional deficiencies, food allergy and intolerance, digestive dysfunction, abnormal gut flora (microbiome) and infectious issues are often part of the total evaluation of the person with chronic fatigue. Here is the complete list.
- Poor dietary habits
- Inadequate exercise
- Insomnia and sleep disturbance
- Thyroid and other hormones including sex hormone deficiency-estrogen and progesterone in women and testosterone and DHEA in men and women
- Nutrient deficiency (B vitamins, especially B12, magnesium),
- Mitochondrial dysfunction- poor diet, alcohol excess and unique genetic nutrient requirements
- Food allergy and gluten intolerance and inflammation
- Digestive issues- malabsorption, leaky gut and microbiota dysbiosis
- Infections (Lyme, EBV,CMV)
- Chronic Fatigue Syndrome
- Mold and other allergies
- Heavy metals (lead, mercury, cadmium) and other toxins
- Major depression and anxiety disorders
- Inflammation from poor diet, stress, lack exercise
- Stress and poor adaptation, adrenal fatigue/dysfunction and allostatic load
Each of these problems is treatable with the appropriate evaluation and both natural and hormonal therapies. Let’s start with the adrenal fatigue component since in our highly stressed world, it is almost always an aspect of fatigue.
Lab tests needed to assess fatigue
- Salivary cortisol (4 samples)
- Blood cortisol and CBG levels, urinary measures of cortisol
- TSH, free T4, free T3, thyroid antibodies, reverse T3
- Hormone evaluation -DHEA, testosterone, estrogen,pregnelone
- CMP, CBC and other routine blood tests
- Vitamin and mineral levels with blood levels and urine organic acid tests
- Comprehensive stool exams to evaluate the microbiota and digestive functions
- Allergy tests for food intolerance (provocative-neutralization intradermal testing)
- Heavy metal testing with provocation
- Genetic tests for metabolic mutations (SNP’s)
Example salivary cortisol test results
Treatment for Chronic Fatigue
With my practice experience spanning four decades I have found what works for each person in treating fatigue. Anyone with a chronic issue needs the comprehensive assessment I outlined above and an integrated therapeutic approach that includes many of the following areas.
Thyroid and other hormone optimization
The most common hormone issue with fatigue, other than cortisol, is low thyroid function. Most physicians do not measure all the needed blood tests (reverse T3, thyroid antibodies, free T3), look for signs on physical exam or listen to the patient for clues about under-functioning thyroid. Symptoms of functional hypothyroidism (which can be present even with normal blood tests like the TSH) are:
- Fatigue
- Weight gain
- Dry skin
- Constipation
- Poor concentration and short term memory
- Menstrual irregularities
- Hair changes -brittle or hair loss.
- Low body temperature and cold intolerance
Thyroid problems can occur at any age, often after stress or viral illness, which can lead to thyroiditis (Hashimotos), found in almost 10% of women. Treatment with whole thyroid extracts (Naturthroid ™ , Armour Thyroid ™ ) can make an enormous difference in fatigue and other symptoms.
Normalizing other hormones especially DHEA, pregnenelone, and the sex hormones, estrogen and progesterone in women and testosterone in men and women can be an answer to fatigue as well. Appropriate testing is the first step as well as assessing symptoms and use age specific bio-identical hormone therapies can make a world of difference.
Intravenous and intramuscular vitamins
For some of my patients we use injectable or intravenous vitamins to jump start the repair process. This powerful treatment brings the nutrients needed directly to the cells by creating a high gradient in the blood which provides the key minerals and vitamins required for optimum function. Included in the IV therapy are high dose vitamin C, minerals including magnesium, zinc and selenium, B vitamins and anti-oxidants glutathione and taurine. I have been using IV and IM therapies for over 30 years and they often are the key in turning around chronic fatigue.
Read more about intravenous and intramuscular vitamins for fatigue >
Acupuncture for Fatigue
Another potent therapy for fatigue we use at the Moss Center for Integrative Medicine is acupuncture. Studies have shown even in chronic fatigue syndrome (see below) acupuncture both traditional and with electro-stimulation have reduced fatigue in up to 80% of subjects. In my experience, Five Element acupuncture which I use in addition to medical acupuncture can bring a new level of energy through changes in the midbrain, hormonal system and the autonomic and central nervous system. These changes have been documented through functional MRI studies and primarily help to reset the stress and trauma induced dysfunction that leads to adrenal and hormonally triggered fatigue.
Read more about acupuncture treatments for fatigue >
Addressing Food Allergies and Gluten Intolerance for Effects on Fatigue
Fatigue is the most common complaint with food or gluten intolerance, but other issues including digestive symptoms, bloating GERD, IBS, headaches, joint and muscle pain and mood disorders. Food intolerance triggers inflammation in the gut wall and activates an immune response causing inflammation in the whole body.
Through our unique skin testing technique (read more) and cutting edge blood tests many of our patients have improved their low level of energy through diet changes based on the test results. If you have fatigue try an experiment: avoid the key 7 foods most likely to be a problem: wheat, dairy, soy, corn, sugar (all sources), tomatoes and citrus. You should know within 2 weeks if this helps the fatigue. Take a look at my book www.TheAdaptationDiet.com for more details.
Read more about addressing food allergies and sensitivities to treat fatigue >
Diet, Malabsorption and Fatigue
Without the right guidance and evaluation, sifting through all the dietary approaches being promoted for increasing energy can be a daunting task. Let me simplify what is most important:
- Eat plants (only organic) with deep colors, both vegetables and fruits to obtain the phytonutrients needed to reset metabolism.
- Avoid simple sugars (deserts, sweeteners, alcohol) that strip key vitamins and minerals from one’s stores (especially magnesium and B vitamins)
- Get 40-70 grams of high quality protein that is organically raised (free range chicken, wild salmon and other low mercury fish, organic cultured dairy-yogurt, kefir if tolerated) some grass fed beef if desired
- Use high quality fats in large amounts-olive oil, nuts and seeds (raw almonds, walnuts, pumpkin, sunflower seeds), and if needed MCT (medium chain triglycerides) oils
- Limit alcohol and caffeine use to 6 ounces red wine, and 1 cup coffee per day
- Consider 5 small meals a day, normalizing blood sugar swings
- Try to get a 12 hour fast between dinner and breakfast with 3 hours between dinner and sleep
My book,The Adaptation Diet, (www.theadaptationdiet.com) presents a program that will lead to higher energy and improved weight and overall well-being. Take a look.
Malabsorption can greatly complicate matters when fatigue is on-going. Even if one’s diet is great there are times when the gut function interferes with getting the nutrients to the cells leading to fatigue. This occurs for the following reasons:
Hydrochloric acid deficiency from stomach issues or use of over the counter or prescription acid blocking medications (PPI’s, H2 blockers )
Pancreatic enzyme deficiency and bile acid issues
Microbiota imbalance leading to gut wall dysfunction
Inflammatory conditions of the digestive tract
Lack of soluble fermentable fiber (legumes, cherries, garlic, onions) that support beneficial intestinal bacteria which produce short chain fatty acids like butyrate
The key supplements for fatigue
- B12 best used in a sublingual (under the tongue) form 1000 ucg of methylcobalamin
- Folate as methyl tetrahydrafolate (MTHF) 1-2 mg
- B complex with methyl B12, folate, B6 as pyridoxal 5 phosphate 25-50mg
- Magnesium either chelate, glycinate, threonate or citrate, 400-600mg
- Zinc as picolinate 25-50mg
- EPA-DHA (omega 3 fish oil) 1to 3 grams
- L-carnitine, CoQ10, alpha lipoic acid as mitochondrial support (See below)
- Curcumin, ashwaghanda, adaptogenic herbs (see adrenal treatment)
Mitochondrial Dysfunction: An Underlying Reason for Fatigue
Fatigue, whether chronic or intermittent, often has a nutritional basis. Energy is produced by the mitochondria as ATP which cells use as fuel for all metabolic processes, making proteins and other components needed for health. Nutrients such as carnitine, CoQ10 and alpha lipoic acid are the key ingredients in the manufacture of ATP by the mitochondria if they are healthy. In cases of chronic fatigue such as chronic fatigue immune dysfunction syndrome (CFIDS), fibromyalgia and CIRS, even with adequate nutrients there can be underlying mitochondrial dysfunction.
Mitochondrial issues can be triggered by genetics with mutations in key genes that control metabolism, (MTHFR,MTRR, CBS, COMT), viral illness such as CMV, EBV viruses, toxin overload from heavy metals (lead, mercury, thalium, cadmium) and persistent organic pollutants (POP) including PCB, BPA, organophosphate pesticides, and others as well as nutrient deficiency relative to these other issues. The sum of one’s genes, epigenetics (diet, exercise, environmental exposure, stress) and these other factors will determine any one person’s energy level and overall well-being.
Supporting mitochondrial function starts with managing all of the epigenetic factors above and the following nutrient supplements.
- CoQ10 100-300 mg
- Alpha Lipoic Acid 300 as time release if possible
- Acetyl l-Carnitine 100-200 mg
- PQQ 100mg
- Nicontinamide ribosisde 250 mg.
Chronic Fatigue Syndrome
There are approximately 1 million people with CFS in the U.S. However, many people who are chronically tired do not have the condition that is defined as Chronic Fatigue Syndrome (CFS or CFIDS, chronic fatigue immune dysfunction syndrome) In order to be diagnosed with chronic fatigue syndrome, a patient must have severe and chronic fatigue that lasts six months or more, while other medical conditions that could cause the fatigue must be excluded. The fatigue must significantly interfere with work or daily activities.
In addition to prolonged fatigue, patients must have four or more of the following symptoms to be diagnosed with chronic fatigue syndrome:
- Impairment in short term memory or concentration
- Sore throat and swollen, tender lymph nodes, recurrent viral like illness
- Muscle and joint pain
- Non-restorative sleep
- Post exercise fatigue
- anxiety, depression, panic attacks
- Night sweats, chest pain
- Dry eyes, dry mouth
- Irregular heart beat
Many patients I see have have symptoms of severe fatigue but do not meet the diagnostic criteria for CFS set by The Centers for Disease Control (CDC). The CDC estimates that fewer than 20% of people who have CFS are actually diagnosed. Many patients have been told their problem is ‘in their head’. A thorough history and the approach I outlined above often results in recovery.
In my patients with actual CFS, I have found improvement if a comprehensive approach is employed. Looking for underlying causes, dealing effectively with stress, repairing nutritional deficiencies (especially with IV and IM treatment), and acupuncture are often required to assist in recovery from this challenging condition.